Harvard-Trained Pediatrician Starts Her Direct Primary Care Practice in Dallas Texas
Welcome to Episode 6 of the Startup DPC Show, and in this episode we have the pleasure of speaking with Tonya McDonald, MD. Dr. McDonald is a Pediatrician and the founder of Radiance Pediatrics in Dallas, Texas. Dr. McDonald trained at Harvard Medical School, graduating in 1998 and she completed her Pediatrics Residency at Baylor College of Medicine.
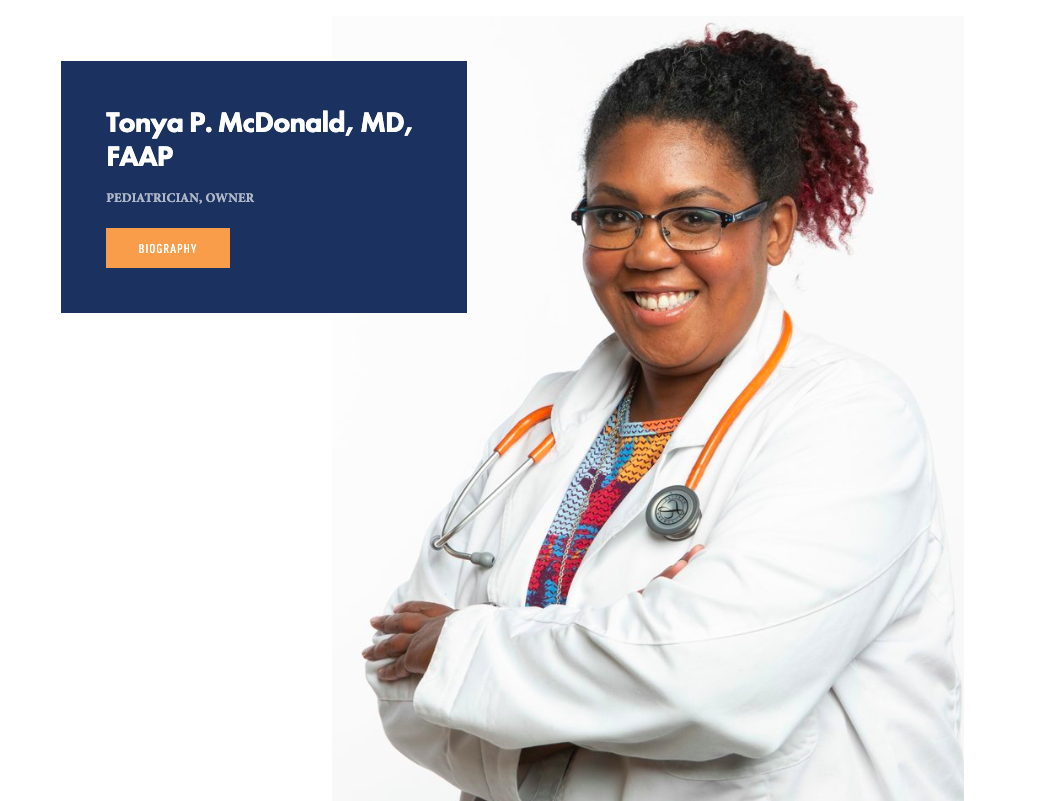
Dr. McDonald is a Pediatrician and the founder of Radiance Pediatrics in Dallas, Texas. Dr. McDonald trained at Harvard Medical School, graduating in 1998 and she completed her Pediatrics Residency at Baylor College of Medicine. She is the featured Direct Primary Care doctor for our Startup DPC Show, Episode 6.
Dr. McDonald was recently interviewed by Harvard Medical School’s Magazine in a section called The New Black Bag. Here’s a segment of the interview:
This past spring, she opened Radiance Pediatrics, a direct primary care practice that provides in-home and virtual pediatric care to families who pay a flat monthly fee. For this fee, families get extended visits, same- or next-day appointments, telemedicine visits, and direct access to McDonald through phone, text, and email.
“In some ways, this is a throwback, an old-school approach to medicine,” she admits. “But it gives me the opportunity to help rebuild the doctor-patient relationship. It’s a gift to be able to truly bond with families.”
Not long ago, McDonald was part of the 78 percent of U.S. physicians struggling to cope with burnout, a problem some have labeled a public health crisis.
“In the past five years, I was seeing up to thirty children a day, feeling sad that I couldn’t practice medicine the way I wanted,” McDonald says. “Insurance dictated what I could do.”
McDonald knew it was time for a change. And she’s far from alone.
As shown in the interview from HMS above, Dr. McDonald is a quintessential physician on the front lines of the healthcare system, dealing with a packed schedule and not having enough time to fully take care of patients. I also love that she says that she now has the opportunity to rebuild the doctor-patient relationship - I put that in bold for emphasis. Now that we have some context, let’s jump into the interview!
Dr. McDonald’s Startup DPC Story
Dr. McDonald had heard about direct primary care ten years ago, but put it in the back of her mind. Three years ago, while working for Children’s Hospital of Dallas, she got tired of seeing 24, 25, or 30 high-risk pediatric patients each day. This was especially difficult when she was taking care of high-risk, high-needs children with complicated medical problems and adverse social determinants of health. Having only 10 minutes for these patients didn’t work for Dr. McDonald.
The final straw was when her pediatric group was “restructured” to an even higher volume practice with multiple physician extenders in the group. She was laid off, took a severance package, and started planning her transition into direct primary care.
Caring for an underserved community with Direct primary care
Dr. Tonya McDonald is serving pediatric patients and families on the south side of Dallas. Dr. McDonald states that there’s a lot of money in Dallas, but most of that wealth is concentrated in Downtown or on the North Side of the city. She goes on to say that the south side of Dallas has a majority minority population - about 40% African American and 30% Hispanic. The median income in the community is roughly $55,000 each year. She alludes to the historical context of living in the south with restrictive housing covenants, which accounts for income inequality and segregation in this area. Dr. McDonald wants to serve in this type of community because she’s a black, female Pediatrician and she enjoys taking care of people in this population. She also alludes to making an impact by being a role model for kids who may not be able to see a black pediatrician, and she also discusses how it’s empowering to serve in a medically underserved community.
Photo of Dr. Tonya McDonald making a house call, courtesy of Harvard Medical School’s a New Black Bag series.
How Direct Primary Care can Address Health Disparities
Dr. Tonya McDonald discusses how some people hear about a “members only” clinic and think that it’s exclusively for the rich. On the contrary, she takes care of folks who are truly in the middle - these are the folks that make too much to qualify for Medicaid or Children’s Health Insurance Program (CHIP) but they don’t make enough to afford private insurance. These patients are willing to save up and cash pay for their healthcare services, but they didn’t have access to affordable options. Now that Dr. McDonald is in the market, these families now have that option to save up and cash pay for an affordable, accessible pediatrician. These families understand the value of direct primary care and the cost savings therein.
How much does a pediatrics direct primary care membership cost?
For Dr. Tonya McDonald and her Radiance Pediatrics practice in Dallas, she charges a monthly membership that costs $125 per month for children from birth to 2 years of age, $100 per month for children 2 years of age to 15 years of age, and $75 per month for adolescents and young adults from 16 to 26 years of age. She also has some discounts available.
Membership Fees:
One Time Enrollment Fee: $100 Per Child
Introductory Monthly Fee For First 25 Families:
0-2 Years - $125
2-15 Years - $100
16-26 Years - $75
Discounts Available: 3 Or More Enrolled Children; Foster Care Children; Full Annual Payment; In-State College Student
Knowing the market when setting your prices
Dr. Tonya McDonald took a look around at the different healthcare costs in the marketplace, namely the costs for home births, doulas, midwives, and similar services. She notes that families in her community were often paying $5,000 to $12,000 for 9 months of care from a midwife and $2,000 to $3,000 for perinatal care from a doula. In that context, paying $100 each month for high-quality, evidence-based pediatric care is not that much money.
“People who value you will pay you what you’re worth.” - Dr. Tonya McDonald
Dr. McDonald also talks about folks in her community who pay $125 for lash extensions plus $75 every 2 to 3 weeks for maintenance of her lashes. In that context, paying $100 each month for high-quality, evidence-based pediatric care is not that much money. She goes on to say that “People who value you will pay you what you’re worth. And those who don’t want to pay you what you’re worth probably wouldn’t pay you consistently for the long term, even if you were half the price because they just don’t value you.”
What are the monthly expenses like for a house call only Pediatric Practice?
Dr. Tonya McDonald works out of a co-working space and she’s surrounded by other entrepreneurs. These folks are smart risk-takers, they’re all about new ideas, and they help her to become a better business person. By renting space at a co-working space, she doesn’t have to use her home address as her business address. She also has storage space for her supplies as a part of her rent, which is $300 per month.
She bought a separate car via her business because it’s easier and cheaper to maintain with commercial insurance. Buying this relatively inexpensive car helps to build credit for her business as well. She buys a lot of her supplies via Henry Schein and Amazon, and she even splits supplies with other local pediatricians. This helps to keep her overhead low.
They are not able to dispense medications in Texas, because it’s not legal for physicians to dispense medications in Texas. This is one of the rare exceptions in the DPC landscape, as virtually every other state in the US allows for physicians to dispense medications from their offices, but not Texas.
Malpractice Insurance is $71 monthly for claims-made coverage. She shopped around and looked at 4 different carriers and also negotiated. She states that as a DPC practice, you have a lower volume, you don’t have 2,000 or more patients, so you should be paying a lower malpractice insurance rate. She expects her malpractice insurance to max out at $300 per month.
What do you do for Pediatric Vaccines in your direct primary care practice?
Dr. McDonald has partnered with some pediatricians in town to purchase single vaccines from their bulk stock. She has a PedsPal account, so she knows how many vaccines she’ll need for the year, and she keeps a log of what she uses and pays the pediatrician for these vaccines. She then bills her patients directly for the vaccine cost, at cost. If her patients are uninsured, she directs them to the county health department for their pediatric vaccines, which are $5 per shot. Finally, children over 7 can get their shots directly from the pharmacy, covered by the insurance with no copays, so she directs families to this option as well. For a few of her patients, she can give the vaccine and bill through VaxCare, which bills the patient’s insurance for the vaccine.
Thank you for reading! To watch the full conversation, see our YouTube video below.
Resources for starting and growing a direct primary care practice
If you’re interested in learning more about starting and growing your direct primary care practice, head over to our courses where you can learn how to attract more patients to your practice, write the perfect business plan, or find the perfect space for your growing DPC practice.
Sincerely, Dr. Paul Thomas